Hentet: https://www.nejm.org/doi/full/10.1056/NEJMoa2309822
Microplastics and Nanoplastics in Atheromas and Cardiovascular Events
Abstract
BACKGROUND
Microplastics and nanoplastics (MNPs) are emerging as a potential risk factor for cardiovascular disease in preclinical studies. Direct evidence that this risk extends to humans is lacking.
METHODS
We conducted a prospective, multicenter, observational study involving patients who were undergoing carotid endarterectomy for asymptomatic carotid artery disease. The excised carotid plaque specimens were analyzed for the presence of MNPs with the use of pyrolysis–gas chromatography–mass spectrometry, stable isotope analysis, and electron microscopy. Inflammatory biomarkers were assessed with enzyme-linked immunosorbent assay and immunohistochemical assay. The primary end point was a composite of myocardial infarction, stroke, or death from any cause among patients who had evidence of MNPs in plaque as compared with patients with plaque that showed no evidence of MNPs.
RESULTS
A total of 304 patients were enrolled in the study, and 257 completed a mean (±SD) follow-up of 33.7±6.9 months. Polyethylene was detected in carotid artery plaque of 150 patients (58.4%), with a mean level of 21.7±24.5 μg per milligram of plaque; 31 patients (12.1%) also had measurable amounts of polyvinyl chloride, with a mean level of 5.2±2.4 μg per milligram of plaque. Electron microscopy revealed visible, jagged-edged foreign particles among plaque macrophages and scattered in the external debris. Radiographic examination showed that some of these particles included chlorine. Patients in whom MNPs were detected within the atheroma were at higher risk for a primary end-point event than those in whom these substances were not detected (hazard ratio, 4.53; 95% confidence interval, 2.00 to 10.27; P<0.001).
CONCLUSIONS
In this study, patients with carotid artery plaque in which MNPs were detected had a higher risk of a composite of myocardial infarction, stroke, or death from any cause at 34 months of follow-up than those in whom MNPs were not detected. (Funded by Programmi di Ricerca Scientifica di Rilevante Interesse Nazionale and others; ClinicalTrials.gov number, NCT05900947.)
The production of plastics is constantly increasing, and this trajectory is set to persist until 2050.1 Plastics can pollute the environment by way of ocean currents, atmospheric winds, and terrestrial phenomena, contributing to their widespread distribution.2,3 Once released into nature, plastics are susceptible to degradation, leading to the formation of microplastics (defined as particles smaller than 5 mm) and nanoplastics (particles smaller than 1000 nanometers). Both types of particles trigger a range of toxicologic effects.4,5
Several studies have shown that microplastics and nanoplastics (MNPs) enter the human body through ingestion, inhalation, and skin exposure, where they interact with tissues and organs.5,6 MNPs have been found in selected human tissues, such as the placenta,7 lungs,8 and liver,9 as well as in breast milk,10 urine,11 and blood.12 Recent studies performed in preclinical models have led to the suggestion of MNPs as a new risk factor for cardiovascular diseases. Data from in vitro studies suggest that specific MNPs promote oxidative stress, inflammation, and apoptosis in endothelial and other vascular cells; animal models support a role for MNPs in altered heart rate, cardiac-function impairment, myocardial fibrosis, and endothelial dysfunction.13 However, the clinical relevance of these findings is unknown. Evidence is lacking to show that MNPs infiltrate vascular lesions in humans or to support an association between the burden of MNPs and cardiovascular disease.
To explore whether MNPs are detectable within atherosclerotic plaque and whether the burden of MNPs is associated with cardiovascular disease, we assessed the presence of these substances in surgically excised carotid artery plaque by means of pyrolysis–gas chromatography–mass spectrometry, stable isotope analysis, and electronic microscopy. We then determined whether the presence of MNPs was associated with a composite end point of myocardial infarction, stroke, or death from any cause.
Methods
STUDY DESIGN
We performed a prospective, multicenter, observational study in which patients were assigned to groups (one group with plaque in which MNPs were detected and one group with plaque in which MNPs were not detected) after enrollment. Patients were recruited from Hospital Cardarelli, Ospedale del Mare, and the University of Salerno from August 1, 2019, to July 31, 2020. Consecutive patients with asymptomatic carotid artery stenosis (as classified by the North American Symptomatic Carotid Endarterectomy Trial14) for whom intervention was indicated were screened for this study. A total of 447 consecutive patients were approached to participate, and 312 agreed to undergo screening. Patients with asymptomatic disease were selected for participation, in order to maximize the chances of surviving the postprocedure period and to minimize interpatient variation in plaque phenotypes.15,16 Baseline clinical examinations were conducted and electronic health records were evaluated to collect demographic, clinical, and therapeutic-intervention data. Blood samples were obtained according to standard procedures after overnight fasting for analysis of biochemical variables. After undergoing carotid endarterectomy, the patients were followed to monitor the incidence of nonfatal myocardial infarction, nonfatal stroke, and death from any cause until July 1, 2023. Follow-up visits were according to common clinical practice and were not scheduled. Participants without visits during the follow-up period were considered to be lost to follow-up. Events were adjudicated by means of review of electronic health records by investigators who were unaware of the results of pyrolysis–gas chromatography–mass spectrometry (and thus to group assignments). The protocol was approved by the local ethics review committee (Università Vanvitelli Caserta). The participants provided written informed consent, and we adhered to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines checklist for reporting of data.17
Specimens of the atheromatous plaque that were surgically excised from the carotid artery bifurcation region at atherectomy were collected in glass tubes and then frozen in liquid nitrogen, fixed in 10% buffered formalin, or fixed in 2.5% electronic microscopy–grade glutaraldehyde for subsequent analyses. The abundance of 11 different MNPs was measured with pyrolysis–gas chromatography–mass spectrometry (a quantitative technique that measures MNPs in combination and does not distinguish between microplastics and nanoplastics), and results were corroborated with the use of electron microscopy and stable isotope analysis (see the Supplementary Methods section and Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). Samples were analyzed as they became available to researchers, who were unaware of outcome data. All the authors agreed to submit the manuscript for publication.
PATIENTS
Patients were eligible if they were 18 to 75 years of age, had asymptomatic extracranial high-grade (>70%) internal carotid artery stenosis, and were scheduled to undergo carotid endarterectomy. Exclusion criteria were evidence of heart failure, valvular defects, malignant neoplasms, or secondary causes of hypertension. Patients with complications in the postoperative period before discharge, who had incomplete data, or who were lost during follow-up were excluded from the analysis.
END POINTS
The primary end point was a composite of nonfatal myocardial infarction, nonfatal stroke, or death from any cause among patients with plaque containing MNPs and patients with plaque that did not contain those substances. Secondary end points included levels of tissue biomarkers interleukin-18, interleukin-1β, tumor necrosis factor α (TNF-α), interleukin-6, CD68, CD3, and collagen in patients with evidence of MNPs as compared with those without.
STATISTICAL ANALYSIS
There were no previous data with which to gauge a sample size. Therefore, an interim analysis that included the first 100 patients was performed to calculate the sample size. We observed that 61 patients had evidence of MNPs in plaque and that such patients had a higher risk of a primary end-point event by a factor of 2.1, than patients without MNPs. Considering an alpha of 0.05, a beta of 0.2, a baseline event rate of 9 events per 100 person-years in the group without evidence of MNPs, and a planned follow-up of 3 years, we calculated a sample size of 246 patients, with the intention of using a proportional-hazards model in the data analysis. We expected a 20% loss to follow-up and adjusted the sample size to 300 patients.
After analysis of atherosclerotic plaque, patients were assigned to one of two groups: patients with evidence of MNPs (having detectable levels of at least one of the two substances) or patients with no evidence of MNPs. The distribution of variables was assessed with the use of the Shapiro–Wilk test. Continuous variables were compared between the two groups with a t-test for normally distributed data, the Mann–Whitney U test for non-normally distributed data, and Fisher’s exact test for categorical variables. Linear regression analyses were performed to estimate the association of the burden of MNPs with plaque markers. Cox regression analysis was used to examine the association between the presence of MNPs within plaque and the incidence of the composite primary end point and was adjusted for age, sex, body-mass index, total cholesterol, high-density lipoprotein and low-density lipoprotein cholesterol, triglycerides, creatinine, diabetes, hypertension, and previous cardiovascular events. A two-sided P value of less than 0.05 was considered to indicate statistical significance. All calculations were performed with the use of SPSS software, version 12. Figures were prepared with the use of GraphPad Prism, version 9.1.2.
Results
STUDY POPULATION AND PLASTICS BURDEN
A total of 312 patients who were undergoing carotid endarterectomy were screened. Of the patients screened, 8 had a stroke or died before hospital discharge, and 47 had incomplete data or were lost during follow-up (Figure 1A). Of the 257 patients who completed a mean (±SD) follow-up of 33.7±6.9 months, 150 patients (58.4%) had a detectable amount of polyethylene in excised carotid plaque, and 31 of those (12.1%) also had a measurable amount of polyvinyl chloride in the carotid plaque. Among patients with evidence of these MNPs in plaque, the mean level of polyethylene was 21.7±24.5 μg per milligram of plaque, and the mean level of polyvinyl chloride was 5.2±2.4 μg per milligram of plaque (Figure 1B).
The patients’ characteristics at baseline are summarized in Table 1. Patients with evidence of MNPs were younger; more likely to be men; less likely to have hypertension; more likely to have diabetes, cardiovascular disease, and dyslipidemia; more likely to smoke; and had higher creatinine values than those without evidence of plastics in excised plaque; the other clinical variables appeared similar in the two groups. There were no apparent differences in the incidence of MNPs according to the geographic areas where the patients lived or the centers where they were enrolled (Fig. S2). No substantive differences were found between the patients who were included in the analysis and those who were excluded with regard to the clinical characteristics of the patients or the prevalence and the levels of detected MNPs (Table S1).
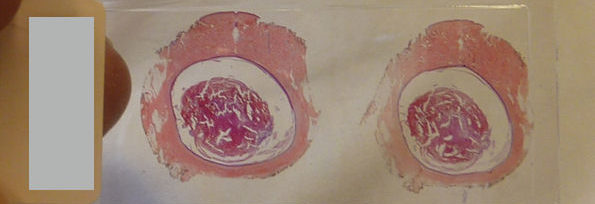
ELECTRONIC MICROSCOPY AND ANALYSIS WITH STABLE ISOTOPES
To substantiate the results obtained with pyrolysis–gas chromatography–mass spectrometry and to gain preliminary information about the size of the MNP particles, we evaluated plaque samples that were positive for both polyethylene and polyvinyl chloride from 10 randomly selected patients using transmission electron microscopy and scanning electron microscopy. Visualization with transmission electron microscopy showed the presence of particles with jagged edges that were probably of foreign origin within the foamy macrophages present in atheromatous plaque and in the amorphous material of plaque (Figure 2A and Fig. S3A). These particles were almost all smaller than 1 μm and were probably nanometers in size.
Observing the same slices using the back-scattered electrons with scanning electron microscopy, we made spectral x-ray maps from some particles that resembled those seen on transmission electron microscopy with regard to size and shape (Figure 2B). These maps provided evidence of a reduction in the presence of carbon and oxygen in the plaque samples and a greater presence of chlorine (Fig. S3B). To compare the elements detectable in the particles with those present in the background, we obtained x-ray spectra from two identical areas and confirmed that the chlorine concentration was higher inside the particles (Fig. S3B). As a further control, we also compared chlorine content in two adjacent identical areas that were devoid of particles and found the levels of chlorine to be similar (Fig. S3C). Given the probable nonbiologic nature of chlorine at the solid state, these results may confirm deposits of polyvinyl chloride. Another example of such particles is shown in Figure S3D; samples from 4 of the 10 patients tested had chlorine levels detectable with this pattern.
Stable isotope analysis was performed on 26 random patient plaque samples because petroleum-derived plastics have lower δ13C values (the ratio of carbon-13 to carbon-12) than human tissues.18 This analysis identified two distinct clusters of patients — one group with higher isotopic values of δ13C and one with lower values — which indicated higher and lower ratios, respectively, of carbon-13 to carbon-12. Lower isotopic values of δ13C could be due to contamination with MNPs, since petroleum-derived material has an isotopic signal lower than that of human tissues. Lower isotopic values of δ13C were more evident in plaque that had evidence of MNPs (Fig. S4).
PLAQUE PHENOTYPE
Because previous data suggested that MNPs can induce proinflammatory pathways,13 four inflammatory markers — interleukin-18, interleukin-1β, interleukin-6, and TNF-α — were measured with the use of enzyme-linked immunosorbent assay (Figure 3A through 3D). Collagen content of plaque samples (Figure 3E) and levels of CD3 (Figure 3F) and CD68 (Figure 3G), two markers of lymphocyte and macrophage infiltration, respectively, were assessed by means of immunohistochemical assay. Linear regression analysis revealed a correlation between the amount of polyethylene present and the expression levels of these markers (Fig. S5). Results of these analyses, stratified according to the presence of polyethylene alone or in combination with polyvinyl chloride, are shown in Figure S6.
CARDIOVASCULAR EVENTS
A primary end-point event (nonfatal myocardial infarction, nonfatal stroke, or death from any cause), occurred in 8 of 107 patients (7.5%) in the group that did not have evidence of MNPs (2.2 events per 100 patient-years) and in 30 of 150 patients (20.0%) in the group that had evidence of MNPs (6.1 events per 100 patient-years) at 33.7±6.9 months. The incidence of individual components of the composite end point is shown in Table S2. Patients with MNPs in plaque had a higher risk of having a primary end-point event than patients with no evidence of MNPs (hazard ratio, 4.53; 95% confidence interval [CI], 2.00 to 10.27; P<0.001) (Figure 4), as shown by Cox regression analysis with adjustment for risk factors for cardiovascular disease (Table S3). The unadjusted hazard ratio was 2.84 (95% CI, 1.50 to 5.40; P=0.007). When the levels of MNPs were analyzed as a continuous variable, the results showed an association with the primary end point (Table S4).
Discussion
Among patients with asymptomatic high-grade (>70%) carotid artery stenosis who were undergoing carotid endarterectomy, those with evidence of MNPs within the carotid plaque had a greater incidence of a composite of myocardial infarction, stroke, or death from any cause than patients who did not have evidence of MNPs within the atheroma. Observational data from occupational-exposure studies suggest an increased risk of cardiovascular disease among persons who are exposed to plastics-related pollution, including polyvinyl chloride, than that seen in the general population.19-21 Mechanistic data from preclinical models has proposed both direct translocation of MNPs into the circulation and indirect mechanisms as possible underpinnings of the cardiovascular toxic effects observed with MNPs, as has been noted with other nanoparticles such as inhaled gold nanoparticles of similar size to MNPs.22 A range of studies in mice and rats showed a wide distribution of MNPs after both inhalation and ingestion, with consistent accumulations in highly vascularized organs and the heart.23,24 Particle size influences the ability of MNPs to reach multiple tissues. According to a World Health Organization statement, MNPs larger than 150 μm or 10 μm in diameter, respectively, are not absorbed into blood and do not penetrate blood vessels.25 Our findings suggest that nanoplastics, rather than microplastics, might accumulate in sites of atherosclerosis. Indeed, the large majority of particles detected in the current study were also below the 200-nm threshold suggested for gut and other barriers and were visible in the extracellular space as scattered debris, which aligns with the notion that the absorption and distribution of MNPs increase as particle size decreases.26 Data from studies in humans have shown that MNPs of up to 30 μm in size have been detected in liver samples, up to 10 μm in placenta samples, up to 88 μm in lung samples, up to 12 to 15 μm in breast milk and urine, and more than 700 nm in whole blood.7-12
Qualitatively, pyrolysis–gas chromatography–mass spectrometry analysis indicated that, among the 11 MNPs tested, polyethylene and polyvinyl chloride were detectable within the carotid plaque in microgram quantities (μg per milligram of plaque). Previous studies that used the same technology showed that polyethylene was found in approximately 25% of the whole-blood samples derived from healthy volunteers, with a maximum concentration of 7.1 μg per milliliter.12 Other studies have suggested that polyethylene and polyvinyl chloride were also the most abundant MNPs found in human breast milk and urine,10,11 with polyethylene fibers observed in human lung tissue at a concentration of 1 particle per gram of tissue.8 The presence of polyvinyl chloride has also been shown in a consistent number of liver samples obtained from patients with cirrhotic disease, in the range of a few particles per gram of tissue.9 Polyethylene nanoplastics have been reported to induce a range of noxious effects on the cardiovascular system in zebrafish embryos, promoting the development of pericardial effusions, the inhibition of angiogenesis, and the induction of a prothrombotic status.27 Similar data are available from studies of the effects of polyvinyl chloride.28 However, in most preclinical studies, high levels of MNPs are assessed — orders of magnitude beyond those observed in the present study, a factor that makes extrapolation of the relevance of preclinical findings to humans difficult.
Polyethylene and polyvinyl chloride, in their various forms, are used in a wide range of applications, including the production of food and cosmetics containers and water pipes. MNPs have been found in drinking water, a large range of foods, cosmetic products, and air, also in a form bound to fine, inhalable particulate matter with an aerodynamic diameter of 2.5 μm or less (PM2.5) and transported long distances by wind.5,6,29,30 Given the wide distribution and availability of MNPs, the attribution of all potential sources in humans is nearly impossible. Our study was not designed specifically to explore the possible sources of plastics underlying the presence of MNPs within carotid plaque. Comparison of data on the basis of the locations of patients’ homes and of the recruitment centers did not reveal obvious differences. Similarly, we cannot establish why only polyethylene and polyvinyl chloride, among the 11 types of plastics assessed, were detected. Studies in animal models suggest that the physicochemical features of different MNPs influence whether they reach distant organs.30,31 Additional work is needed to assess whether polyethylene and polyvinyl chloride accumulate preferentially within plaque and whether they are more pathogenic than other types of MNPs in this regard.
It is important to note that our results do not prove causality. The association between the presence of MNPs within plaque and the incidence of a composite of cardiovascular disease or death outcomes may also entail the risk from exposure to other residual, unmeasured confounding variables, such as unknown exposures during the life course of the patient or, more broadly, the health status and behaviors of the patients. In addition, we did not consider levels of exposure to PM2.5 and PM10, which is an emerging risk factor for cardiovascular disease.31
Our study has limitations. Despite the preventive measures adopted, laboratory contamination cannot be firmly ruled out. Even though we applied updated procedures to collect and analyze plaque specimens, the residual risk of contamination might exist. Future studies performed with the use of clean rooms, where there is no plastic in any form except the material under study, might corroborate our observations. We did not have socioeconomic data available for our study population. Income and education, among other conditions, are linked to a wide range of outcomes and might be particularly relevant.32 Our findings pertain only to a population of asymptomatic patients undergoing carotid endarterectomy, who may not be representative of the general population.14 Thus, our findings may not be generalizable. The representativeness of patients who participated in the study is shown in Table S5. We did not explore the variables of food and drinking water, which may be linked to accumulation of MNPs in humans.25,33,34 Thus, it is possible that the putative role of MNPs in driving cardiovascular disease might be limited if compared with canonical risk factors, given that over a period of decades in which exposure to plastics has presumably been increasing, the rate of cardiovascular disease has been falling.35 However, results of our study show that patients with MNPs that were detected in carotid artery plaque have a higher risk of a composite end point of myocardial infarction, stroke, or death from any cause at 34 months of follow-up.
NOTES
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
Supported by a grant (2020LM8WNW) from Programmi di Ricerca Scientifica di Rilevante Interesse Nazionale (scientific research programs of high national interest) to Dr. Marfella, support from the Italian Ministry of Health–Ricerca Corrente to IRCCS MultiMedica, and grants (1R35ES031702 and R01ES017290) from the National Institutes of Health to Dr. Rajagopalan.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
SUPPLEMENTARY MATERIAL
REFERENCES
1.
Geyer R, Jambeck JR, Law KL. Production, use, and fate of all plastics ever made. Sci Adv 2017;3(7):e1700782-e1700782.
2.
Wang S, Chen H, Zhou X, et al. Microplastic abundance, distribution and composition in the mid-west Pacific Ocean. Environ Pollut 2020;264:114125-114125.
3.
Collignon A, Hecq J-H, Glagani F, Voisin P, Collard F, Goffart A. Neustonic microplastic and zooplankton in the north western Mediterranean Sea. Mar Pollut Bull 2012;64:861-864.
4.
Galloway TS, Cole M, Lewis C. Interactions of microplastic debris throughout the marine ecosystem. Nat Ecol Evol 2017;1:116-116.
5.
Vethaak AD, Legler J. Microplastics and human health. Science 2021;371:672-674.





 Views Today : 41997
Views Today : 41997





